Airborne particulate matter and their health effects
PDF
Airborne particulate matter is one of the main air pollutants. Most of their health effects have now been known for many years. Their impact on mortality, the occurrence of pulmonary and cardiovascular complications, have been the subject of numerous studies. It has also been shown that long-term effects are more serious than short-term effects. Finally, the socio-economic cost of this pollution is considerable and preventive measures are still insufficient.
1. General concepts
Everyone needs breathing to live! This basic truth explains the importance of air quality. Unlike other exposures, such as food, no one can avoid the obligation to breathe! The whole population is therefore concerned; all age groups, whether healthy or sick.
The health effects of air pollution have been studied for several decades. Since the first alerts in the Meuse Valley in Belgium in 1930 and in London in December 1952 when dense fog due to pollution caused several thousand deaths, much progress has been made in understanding the effects of different air pollutants on human health.
Among the many pollutants present in the air, of natural or anthropogenic origin (due to human activity), suspended particles have been the subject of a great amount of work.
1.1. Suspended particles
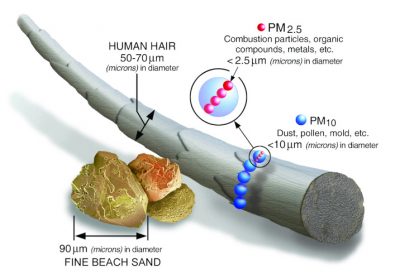
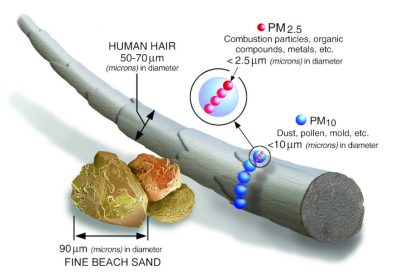
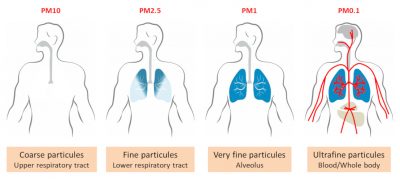
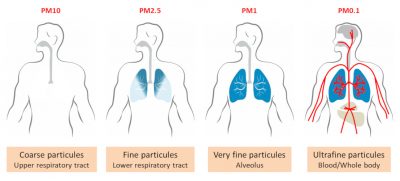
Particulate Matter (PM) particles are classified according to their aerodynamic diameter expressed in µm. The particles that are routinely analyzed in France by air quality monitoring devices are 10 µm in diameter; they are noted as PM10; they are referred to as “coarse” particles. Fine particles are defined as those with a diameter of less than 2.5 µm (PM2.5) (Figure 1). And in recent years, there has been an interest in so-called “ultra-fine” particles, with a diameter of 0.1 µm (or 100 nm), or PM0.1. Nanoparticles, then.
These diameter considerations are fundamental because they condition the penetration of particles into the bronchopulmonary system and into the body (Figure 2). Basically, only PM2.5 and smaller will penetrate deep into the lungs and into the alveoli of the lungs; PM0.1 partially penetrate the body through the alveolar-capillary membrane, which separates air from the blood stream. The reality in humans in vivo is probably much more complex and still partly unknown. Most of the knowledge on the subject comes from mathematical models and some animal experiments.
Particulate air concentrations, PM10 in routine, are measured (a) near or at a distance from the emission source, most often by fixed air quality analysis stations: i.e. near industrial installations, in urban areas, or near a road axis, etc.; or (b) at a given distance from known sources, in order to detect possible pollution peaks while measuring “background noise”. Mobile stations (Figure 3) are also used for spot analysis campaigns, usually remote from emission sources. Fine particles, PM2.5 or PM0.1 are not routinely analyzed, but campaigns for measuring PM2.5 are increasing.

Thus, lowering emissions is obviously highly desirable; this does not necessarily mean that the concentrations of the air we breathe will decrease in the same proportions. This makes it possible to insist on the long-range transport of pollution, particularly fine and ultra-fine particles, by winds and atmospheric masses; and to stress that the air in the countryside is not always obviously better than the air in the city. Even if it is often the case.
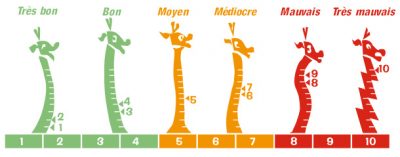
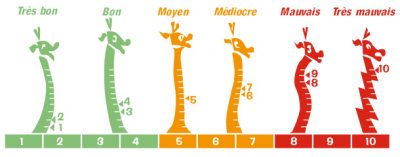
The ATMO index therefore makes it possible to report pollution peaks, due to PM10 for example, as is often the case in winter during high pressure periods, or to ozone in the middle of summer. However, it can be the source of a misunderstanding. It may suggest to the public or to certain authorities that health is only threatened when pollution peaks occur. However, we now know that health is affected by prolonged exposure to airborne particles over the long term and not only during pollution peaks. A pollution peak is therefore only the tip of the iceberg of the health effects of air pollution!
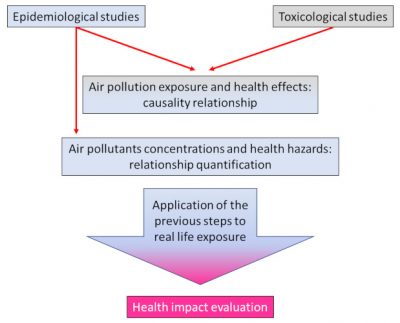
1.2. How to study the health effects of particulate matter?
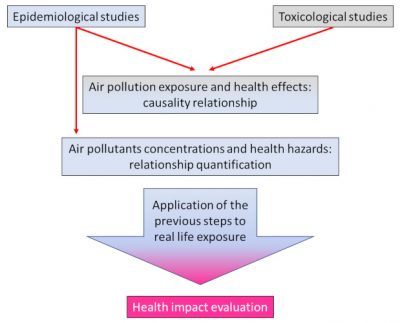
Toxicology makes it possible to study the effects of pollutants on health using mathematical or experimental models, at the cellular, tissue or sometimes animal level. Under rigorous conditions, the effect of a specific pollutant on a particular organ can be studied and a so-called risk assessment conducted. The ultimate objective of risk assessment is to compare the level of risk measured in the laboratory with the level of risk to which we are exposed in reality, by studying and quantifying the exposures to which we are exposed (exposure scenarios). It is on the basis of these studies that scientists propose “standards” to the health authorities, i.e. in general concentration thresholds that should not be exceeded.
The “construction” of standards is relatively simple when a threshold for the appearance of effects has been detected in the laboratory; with the application of a number of factors known as “uncertainty factors”, a “threshold” -the standard- can be proposed for humans. Things get more complicated when no threshold has been detected: the substance is toxic at the lowest doses. This is the case for most air pollutants, including particulate matter. It is therefore important to understand that in terms of air quality, “regulatory” standards are concentration thresholds estimated by modelling for a so-called “acceptable” risk. These standards are therefore always to be considered as provisional and as the “least bad” possible. And as we have to breathe, so there is no such thing as a Zero risk [2].
Epidemiology, i.e. the study of the relationships between diseases and factors likely to influence their frequency, distribution and evolution, evaluates the consequences of air pollution on the scale of a population, a city, a region, a country, etc. [3].
Two main methods are used in epidemiology to study the health effects of air pollution, time series and cohort studies.
Cohort studies will provide long-term, multi-year results. A cohort is a population of subjects who meet a specific definition and are monitored over time. These studies therefore consist of following a large number of people, several thousand, for years, taking into account their habits, their private and professional environment, their medical status, etc., and recording all events occurring during the study, such as the occurrence of a disease for example. These are so-called prospective studies that require significant human and financial investment.
Other studies may be conducted such as case-control studies or cross-over case studies. These are retrospective studies. In the case-control study, a group of sick subjects is compared to a group of healthy subjects, looking for one or more factors explaining the disease. In the crossover case study, the subject is his or her own witness, and the aim is to explain the changes over time. With regard to the study of air pollution and taking into account the variety of effects observed in humans, these studies do not have the robustness of cohort studies and are less common.
Epidemiology also makes it possible to measure what is called “relative risk“. It is the relationship between the incidence of a disease occurring in subjects at risk and the incidence of the disease in subjects not at the same risk (incidence is the frequency of new cases of a disease over a given period, such as a year). We are talking about high and low risks. For example, for active smoking, the relative risk is about 30; i.e. the probability of developing lung cancer is 30 times higher when you smoke than when you don’t smoke. Air pollution is considered a “low” risk, less than 2, and it is important to understand the meaning of this term: the probability of effects occurring is lower, but the effects are just as serious when they occur. This lower probability of effects occurring explains the absolute need to include several thousand subjects in a study in order to observe them and obtain meaningful results.
Finally, the statistical method is applied in all cases and its main objective is to eliminate any results that could be due solely to chance. Assuming that we want to study the effects of air pollution on all French people. Can a cohort study be conducted by following more than 66 million people over the years? No, of course not. A “representative” sample will therefore be selected by lot, respecting the diverse composition of the population; the statistical method will make it possible to validate or not the results obtained. Statistical tests make it possible to establish a “significant” relationship between air pollution and health effects. But it is also necessary to establish a real causal relationship [5] between particulate matter and health effects and not just a simple statistical correlation [6] : as discussed by Dab et al. in 2001 [7], the methodology of most of the available studies allows this causal relationship to be established. Among the most frequently used criteria [3] are consistency and reproducibility – effects are constant and reproducible, temporality – exposure-time of effects is consistent, a dose-response effect (this depends on the toxicant involved), and biological plausibility – there is consistency between known mechanisms of toxicity and observed effects.
2. Mechanisms of action
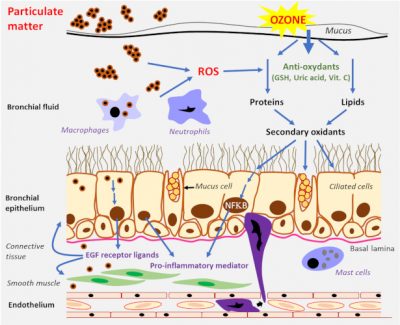
Toxicological studies at the cellular level and in animals have contributed to a better understanding of the mechanisms of action of particles on the body. They have largely explained the relationships demonstrated by epidemiological studies between particulate matter and health effects [8].
Fine and ultrafine particles are known as respirable particles because they settle in the lungs to the alveoli. It has been shown that particulate deposition in the lungs is higher in patients with obstructive bronchial diseases such as asthma and chronic obstructive bronchopathy. Particulate matter deposition is heterogeneous across lung areas and there is a high degree of inter-individual variability. A small fraction of the ultrafine particles can pass into the bloodstream and secondarily reach other organs [9].
Another potential pathway for ultrafine particles is the olfactory pathway; this pathway, known for some viruses, could allow ultrafine particles to reach the brain [9]. As mentioned above, the digestive and cutaneous penetration pathways are still being studied with incomplete or contradictory results.
The pathogenicity of particles is determined by their size, chemical composition, origin, solubility and ability to produce activated oxygen species. The chemical composition of particles, which varies greatly, partly determines their biological reactivity (see Air pollution particles: what are they?). For the finer ones, some components are to be taken into account particularly, polycyclic aromatic hydrocarbons and quinones on the one hand, and metals on the other hand. Given this complex composition of particles, it is still difficult at present to establish precise causal links between individual particle components and health effects. It has been shown that ultrafine particles have a higher biological reactivity than larger particles. Indeed, and although they constitute a small mass of particles, they are more numerous and will represent, in a given volume, a larger reactive surface.
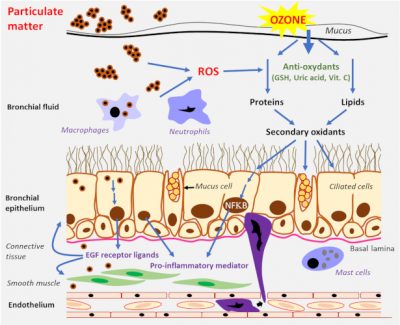
As mentioned above, the composition of particles is one of the determinants of their toxicity. Thus, transition metals [10] such as iron, copper or vanadium, can lead to the production of the highly reactive hydroxyl radical. Organic compounds cause the production of ROS in macrophages and bronchial epithelial cells via quinones and polycyclic aromatic hydrocarbons.
A “Trojan horse” effect has also been described, when particles bind to biological particles or molecules such as bacteria or allergens.
3. Health effects of particulate matter
There are many studies on the health effect of PM and it would be impossible to mention them all. These are most often studies involving tens to hundreds of thousands of subjects.
3.1. Mortality
Mortality studies are the most numerous. Mortality data on a country-by-country basis are readily available and death is a good “marker” of potential environmental health effects. All causes of death, whether “natural” or not, have been investigated in relation to exposure to particulate matter.
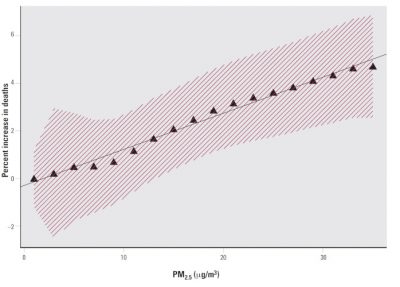
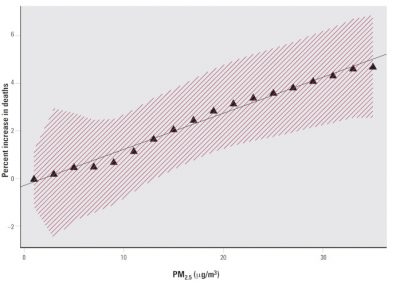
Short-term studies have shown an increase in the number of deaths related to pollution episodes [11],[12],[13],[14]. The most studied particles were PM10 and PM2.5. Large North American studies such as the National Morbidity, Mortality and Air Pollution Study (NMMAPS) conducted in 90 major cities between 1987 and 1994 have shown a weak but consistent relationship between PM10 and death rates. In Europe, the PPHEA and APHEA2 (Air Pollution and Health Effects, a European Approach) studies have produced the same results with PM10. The APHENA study, by combining North American and European results, confirmed the robustness of the study methods and results. Studies on the effects of ultrafine particles (PM0.1) are still few in number but are moving in the same direction.
All cohort studies have also shown an increase in long-term mortality from exposure to particulate matter, particularly PM2.5, since the 1990s [6],[15]. All causes combined, with cardiovascular and cardiopulmonary causes predominating. One example is the European ESCAPE study (Europe Study of Cohorts for Air Pollution Effects), which included 22 cohort studies and more than 300,000 subjects [16], [17]. Another study studied the 12-year impact on the death rate of the main atmospheric pollutants, based on concentrations measured throughout metropolitan France [18]. This study confirms the relationship between pollution and long-term death, even at relatively low concentrations; particulate matter (PM10 and PM2.5 in the study) is the main cause, ahead of nitrogen oxides and ozone.
Many studies have also shown that a decrease in exposure leads to a reduction in the death rate. This is particularly important to note since it has long been thought that only acute episodes of pollution lead to an increased risk to health. It is now known that long-term effects are real and probably more important than short-term effects; this has implications for emission reduction measures and health standards. All studies also show a relationship between particles and mortality even in healthy people; this point, which has been the subject of expert debate, with some thinking that only “fragile” people were at risk, is now a consensus. Nevertheless, some subgroups could be identified as even more at risk: diabetics, people with a history of myocardial infarction, the elderly and people of low socio-economic status.
These results are consistent with European and international estimates. For example, the European Environment Agency estimated in its 2018 report [20] that 35,800 premature deaths [21] are due to exposure to PM2.5 each year in France, a much higher figure than the impact of nitrogen oxides and ozone. This figure is 391,000 for the European Union as a whole (28 countries). The WHO estimates that about 7 million people die each year worldwide from exposure to fine particles. [22]
In summary, all short and long-term studies show a significant causal relationship between particle exposure and mortality.
3.2. Lung disorders
Given the pulmonary penetration of the particles, their pulmonary effects may appear to be the most intuitively expected. Again, the number of studies on this subject is considerable [6]. The majority of studies include PM10 and PM2.5; few studies include PM 0.1, but their results are similar.
Much attention has been focused on young children; their lungs are still immature and their immune systems are still evolving. In addition, children have a higher ventilation per minute than adults and are often involved in outdoor activities. It is also known that lungs condition of young children is a good prognostic factor for the lungs condition in adulthood. Despite heterogeneous results and some interpretive bias, the majority of short-term studies show a relationship between PM2.5 exposure and the occurrence of lung disease and asthmatic disease. It is also recognized that asthmatic children are much more sensitive to the effects of particles than healthy children. Long-term studies confirm a relationship between fine particles and lung function, lung development, and the occurrence of respiratory symptoms.
It has also been shown that an improvement in air quality leads to a decrease in the frequency of hospital admissions and respiratory diseases for children. Fewer studies have been conducted in adults, but all show the occurrence of pulmonary effects related to exposure to particles, in particular the development of chronic obstructive bronchitis.
The occurrence of lung cancers related to air pollution, and fine particles in particular, is now the subject of a scientific consensus. The carcinogenicity of air pollution and particulate matter to humans was recognized by the WHO International Agency for Research on Cancer (IARC) in 2013 [23].
3.3. Cardiovascular diseases
Perhaps unexpectedly, the cardiovascular system seems to be most at risk because of air pollution and fine particles. All Cardiology societies regularly warn of the increased risk of heart disease due to pollution. A good number of short-term studies have thus shown a very significant relationship between exposure to particulate matter, PM10 and PM2.5 and the frequency of hospitalizations for cardiovascular reasons.
Long-term studies have focused in particular on the occurrence of heart failure or myocardial infarction. Other studies have focused on more modest changes in cardiac physiology, such as changes in heart rate or the development of transient myocardial ischemia, but these changes are often indicative of more severe complications. However, given their implementation difficulties, such studies provide fairly heterogeneous results, as no study can definitively conclude. However, all of them clearly converge towards the existence of harmful effects of particles on the cardiovascular system.
As we have seen previously, one of the mechanisms of action of particles is inflammation. This effect is most likely to cause vascular vasoconstriction and the possible development of high blood pressure. But the results of studies on high blood pressure and particles are mostly insignificant and sometimes contradictory; here again the “definitive” study, the one that would allow us to conclude, does not exist.
With regard to ultra-fine particles, and even if the majority of experts are in favor of a PM0.1 relationship and cardiovascular effects, too few studies are currently available to conclude.
3.4. Neurological disorders
A few short-term studies have shown a relationship between fine particles and the occurrence of stroke, particularly ischemic stroke, after an acute episode of pollution. Too few long-term studies are available to conclude on this subject.
A small number of studies have examined the occurrence of neurodegenerative disorders and long-term cognitive disorders. We know that inflammatory processes play an important role in the development of Alzheimer’s disease or Parkinson’s disease. The very first studies were carried out on an animal model of wild dogs living in particularly polluted environments in Mexico; brain lesions of inflammatory origin were detected in these dogs. Although some studies in humans suggest a similar relationship between particle exposure and neurodegenerative diseases, it is still early to conclude definitively.
3.5. Reproductive disorders, perinatal disorders
In 2005, WHO had already drawn attention to the effects of air pollution on the course of pregnancy and the fetus. The responsibility of air pollution, and particles in particular, on the occurrence of premature births, low birth weights, fetal anomalies, infant mortality has been shown by some studies. But we know that the sensitivity of the fetus varies according to the period of pregnancy and this makes it difficult to compare studies. Other interpretive biases such as socio-economic status were discussed. It is also difficult to conclude that there are possible long-term effects of fetal exposure during pregnancy. Even if a bundle of arguments makes the particles responsible for deleterious effects, it is currently impossible to conclude definitively.
3.6. Biological markers
Many short-term studies have attempted to establish a relationship between certain biological blood parameters, markers of inflammation and coagulation in particular, and exposure to fine particles. The most well-known are CRP (C-reactive-protein, marker of inflammation), leukocyte count (white blood cells), red blood cell count and hemoglobin count, fibrinogen count, etc. It is tempting to try to find THE easily measurable blood marker that would indicate exposure to particles. Although some markers of inflammation appear to be related to particle exposure, the results are too fragmented and heterogeneous to conclude.
In summary, the biological marker of exposure to particulate matter, if any, has not yet been identified. Studies are ongoing and advances in analytical techniques will undoubtedly make it possible to make progress on this subject in the coming years.
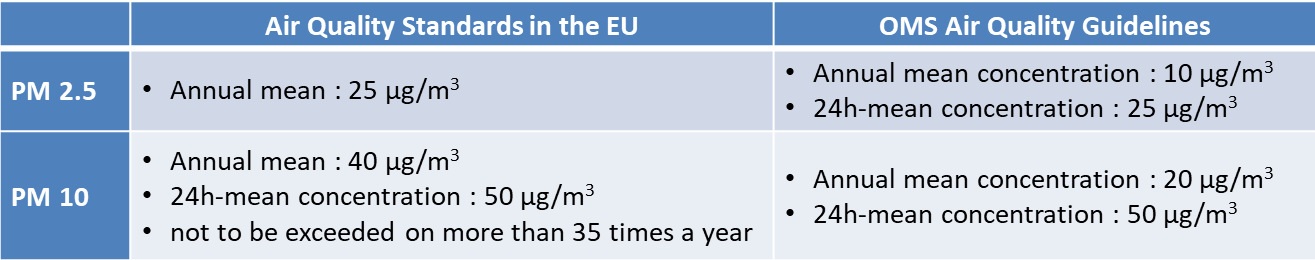
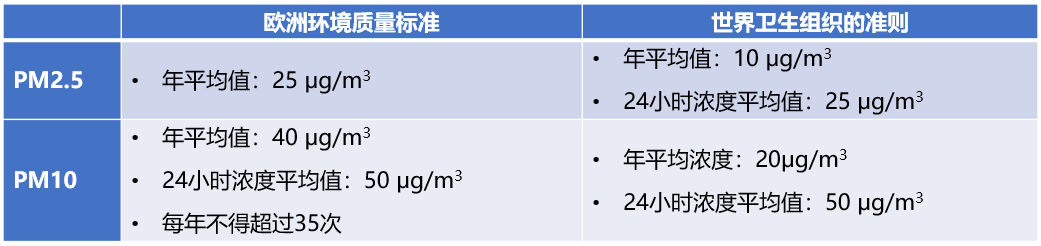
4. Health standards
Health standards are, as indicated at the beginning of this article, the result of estimates and modelling. They are not the same all over the world [24].
It can be noted that the WHO guidelines values are much more protective than the European standards. Many urban areas in France regularly exceed European air quality standards. A rather strict report by the European Court of Auditors pointed to the inadequacy of pollution reduction measures and non-compliance with health standards in several countries, including France. [25]
Information and recommendation thresholds, [26] as well as an alert threshold [27], exist in France for PM10; respectively 50 µg/m3 and 80 µg/m3. It was estimated in 2017 that if all municipalities in France complied with the WHO guideline value for PM2.5, about 17,712 deaths would be prevented and the associated economic benefit would be in the order of 53 billion euros [28].
5. Socio-economic cost
A senatorial commission of inquiry into the economic and financial cost of air pollution estimated it in 2015 at a total of between 70 and 100 billion euros [29]. The cost of air pollution alone to the French health system is estimated each year at between €1 billion and €2 billion, plus expenses relating to pensions paid for occupational diseases amounting to €1 billion. The costs of loss of well-being for society, caused by pathologies and premature deaths, are more difficult to quantify precisely; the range of estimates is quite wide, reaching a maximum of 100 billion euros.
In 2018, the Senate Working Group on Air Pollution recalled that air pollution is a health emergency and a major socio-economic issue.
Most specialists agree that the costs of implementing drastic pollution reduction measures would be much lower than the socio-economic cost of the same pollution. Janez Potocnik, former European Commissioner for the Environment (2009-2014) and a strong advocate of pollution reduction measures, can be quoted in this regard: “If you think the economy is more important than the environment, try to hold your breath while you count the money” [17].
6. Messages to remember
- No one disputes the health effects of air pollution
- Among the various air pollutants, fine suspended particles are the main cause of the health effects of pollution.
- The harmful effects of pollution peaks have long been emphasized. We now know that long-term pollution is probably even more serious than peak pollution levels.
- The causal relationship between particle exposure and mortality has been formally established by a large number of studies. The same is true for pulmonary and cardiovascular effects.
- Neurological effects, effects on pregnancy and reproduction are still the subject of many studies. Some studies already indicate a probable effect of particles, without being able to conclude definitively yet.
- PM10 and PM2.5 particles have been the most studied. A considerable field of research is open to study the effects of PM0.1 nanoparticle.
- The socio-economic cost of air pollution is considerable.
- Too many countries, including France, do not comply with current European air quality standards.
References and notes
Cover image. [Source: © Renée Grillot]
[1] Thompson JE (2018). Airborne particulate matter. Human exposure and health effects. Journal of Occupational and Environmental Medicine, 60, 5 : 392-416.
[2] www.who.int/fr/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health
[3] Ledrans M (2008). L’épidémiologie, un outil pour la veille et la décision en santé environnementale. Environnement, Risques & Santé, 7, 21-26. (in french)
[4] Bias of confusion: one or more phenomena other than the one studied may explain the disease. This bias must be taken into account in the study.
[5] Causality: Exposure to fine particles has many health effects
[6] Correlation: two phenomena evolve in parallel but without being able to formally establish that one leads to the other
[7] Dab W. et al. (2001) Pollution atmosphérique et santé : corrélation ou causalité ? Le cas de la relation entre l’exposition aux particules et la mortalité cardio-pulmonaire. Journal of the Air & Waste Management Association, 51, 2013-218. (in french)
[8] Marano F. (2012). Mécanismes d’action des particules atmosphériques fines et ultrafines. Pollution atmosphérique (numéro spécial), 20-22. (in french)
[9] Baeza A (2007). Pollution atmosphérique et maladies respiratoires, un rôle central pour le stress oxydant. Médecine Sciences, 23, 497-501. (in french)
[10] https://en.wikipedia.org/wiki/Transition_metal
[11] Rückerl R. et al. (2011) Health effects of particulate air pollution: a review of epidemiological evidence. Inhalation Toxicology, 23 (10), 555-592.
[12] Kim K.-H. et al. (2015). A review on the human health impact of airborne particulate matter. Environment International, 74, 136-143.
[13] Kelly FJ et al. (2015). Air pollution and public health : emerging hazards and improved understanding of risk. Environ Geochem Health, 75, 631-649.
[14] Atkinson RW et al. (2014) Epidemiological time series studies of PM2.5 and daily mortality and hospital admissions : a systematic review and meta-analysis. Thorax, 69, 660-665.
[15] Burnett R et al. (2018) Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proceedings of the National Academy of Sciences of the USA, 115 (38), 9592-9597.
[16] Beelen R et al. (2014) Effects of long-term exposure to air pollution on natural-cause mortality : an analysis of 22 European cohorts within the multicentre ESCAPE project. Lancet, 383, 785-795.
[17] Mannucci PM et al. (2015) Effects on health of air pollution : a narrative review. Internal Emergency Medicine, 10(6), 657-662
[18] Sanyal S et al. (2018) Long-term effect of outdoor air pollution on mortality and morbidity : a 12-year follow-up study for metropolitan France. International Journal of Environmental Research and Public Health, 15 (2487), 1-8
[19] Pascal M et al. (2016) Impacts de l’exposition chronique aux particules fines sur la mortalité en France continentale et analyse des gains en santé de plusieurs scénarios de réduction de la pollution atmosphérique. Saint-Maurice : Santé publique France ; 158 p. (in french)
[20] https://www.eea.europa.eu/publications/air-quality-in-europe-2018
[21] Premature death: death occurs before the expected age of death, taking into account the life expectancy of the country concerned. Death that can be prevented if its cause is removed.
[22] https://www.who.int/fr/news-room/detail/02-05-2018-9-out-of-10-people-worldwide-breathe-polluted-air-but-more-countries-are-taking-action
[23] CIRC monography (2013) The carcinogenicity of outdoor air pollution. Lancet, 14, 1262-1263
[24] Annesi-Maesano I (2017) The air of Europe : where are we going ? European Respiratory Review, 26, 1-5
[25] Special Report No 23/2018: Air pollution: our health is still not sufficiently protected. European Court of Auditors. https://www.eca.europa.eu/Lists/ECADocuments/INSR18_23/INSR_AIR_QUALITY_EN.pdf
[26] Information and recommendation threshold: a level of concentration of polluting substances in the atmosphere above which short-term exposure poses a risk to the human health of particularly sensitive groups in the population requiring immediate and adequate information
[27] Alert threshold: a level of concentration of polluting substances in the atmosphere above which short-term exposure poses a risk to the health of the general population or environmental degradation that warrants emergency response.
[28] www.amse-aixmarseille.fr/actualite/pollution-de-lair (in french)
[29] Sénat 2015 « Pollution de l’air : le coût de l’inaction ». Rapport n° 610 (2014-2015) by Mrs Leila AÏCHI, made on behalf of the EC economic and financial cost of air pollution, submitted on 8 juillet 2015. (in french)
The Encyclopedia of the Environment by the Association des Encyclopédies de l'Environnement et de l'Énergie (www.a3e.fr), contractually linked to the University of Grenoble Alpes and Grenoble INP, and sponsored by the French Academy of Sciences.
To cite this article: DANEL Vincent (August 16, 2019), Airborne particulate matter and their health effects, Encyclopedia of the Environment, Accessed September 19, 2024 [online ISSN 2555-0950] url : https://www.encyclopedie-environnement.org/en/health/airborne-particulate-health-effects/.
The articles in the Encyclopedia of the Environment are made available under the terms of the Creative Commons BY-NC-SA license, which authorizes reproduction subject to: citing the source, not making commercial use of them, sharing identical initial conditions, reproducing at each reuse or distribution the mention of this Creative Commons BY-NC-SA license.