Covid-19: pandemic or syndemic?
PDF1. A pandemic, yes, but..
It soon became apparent that this respiratory virus manifested itself differently according to age and “co-morbidities“. Consequently, it seemed legitimate to question the relevance of the medical paradigm that guided – and still largely guides – the strategy for dealing with this pandemic. This paradigm is that of a biomedical approach, mainly supported by epidemic modelers, infectious disease specialists and resuscitators, and doctors specializing in the functions affected (pneumology, cardiology, gastroenterology, etc.). The latter saw Covid-19 as an absolute emergency that had to become the almost exclusive priority of public authorities, to the possible detriment of all other health determinants.
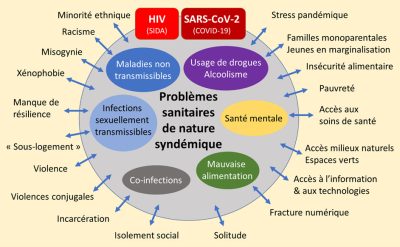
The notion of “syndemia” was coined in 1990 by the American anthropologist Merrill Singer [2], who describes it as “an interweaving of interacting and mutually aggravating diseases“. This new concept of syndemia(Syn in Greek means “together”) was studied in the USA, exploring the interactions between HIV-AIDS, ethnic groups, substance abuse and childhood or partner violence [3]. Thus, a syndemia occurs when risk factors or comorbidities intermingle and potentiate, exacerbating the damage of a disease. Recently, the term “syndemia” has been redefined by Singer et al [4] as “the aggregation of two or more diseases or health problems in a population for which there is some level of deleterious biological or behavioral interface that exacerbates the negative effects of each of the diseases involved“.
A syndemic disease is therefore the global emergence of (i) processes or mechanisms by which diseases interact with each other, the socio-environmental conditions involved and the way in which they translate into circumstances of adversity. (ii) processes or mechanisms by which socio-environmental conditions affect biology and psychology (Figure 1).
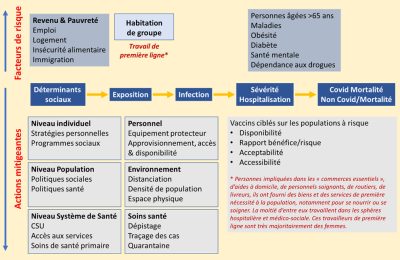
In the context of Covid-19, two categories of disease interact in specific populations: (i) infection with SARS-CoV-2 and (ii) a range of non-communicable diseases (obesity, cardiovascular and respiratory pathologies, cancers) – to which is added a risk factor in our society of ever-increasing life expectancy: age. Consequently, the syndemic nature of the threat we face means that a more nuanced approach is required if we are to protect the health of our communities.
As Richard Horton and others have pointed out, the Covid-19 pandemic became an extreme form of syndemic in a pandemic context: a “pan-syndemic” revealing societal fault lines, where clusters of inequalities, not limited to health, were highlighted by the virus and reinforced by the management of the health crisis, all in a context of growing environmental predation. This was confirmed by a study also published in the Lancet on October 17, 2020: “The interaction of Covid-19 with the steady global rise over the past 30 years in chronic diseases and their risk factors, including obesity, hyperglycemia and air pollution, has created the conditions for a storm, fuelling the Covid-19 death toll.” And the scientists behind the study add that “many of the risk factors and non-communicable diseases studied in this report are associated with an increased risk of severe forms of Covid-19, and even death“.
2. What lessons can be drawn for clinical intervention and teaching?
The lessons to be learned for clinical intervention and teaching are as follows:
- In terms of vaccine interventions: e.g., target vaccination on the most fragile, move to rural areas among the elderly and the less connected.
- We need to combine a driving and supportive role for biomedical initiatives and innovations with a firm commitment to reducing social inequalities and poverty, and improving access to education.
- We need to integrate modern modeling approaches into a multi-disciplinary approach integrating social and environmental sciences [6].
- Take multi-disciplinarity into account in scientific councils, at the level of independent agencies whose missions are governed by the public health code: Santé publique France, Haute Autorité de santé (HAS) and the Haut Conseil de la santé publique (HCSP). Some aspects were discussed in Senate Report no. 199, submitted to the President of the Senate on December 8, 2020 [7].
- Implement the “One Health for All” approach and develop the issues of climate/life/pollution interaction;
- Focus on “sustainable health” systems and their ability to anticipate and predict disruptive events.
- Decompartmentalize lessons to better understand how the pieces fit together, and find out why a more integrated understanding of health and social conditions was the best defense against the next pandemic (which will happen).
For the WHO, health is a “state of complete physical, mental and social well-being and not merely the absence of disease or infirmity“. This is why it is now important to put this holistic approach to health back at the heart of the syndemic management strategy, which cannot be summed up in the absence or presence of Covid-19 alone. The Covid-19 pandemic is, of course, a tragedy. However, if we try to think of it as a “syndrome”, it is possible to draw from this drama a truth and a horizon for the future: our bodies are weakened by our lifestyles; more than health policies to combat disease, we need policies capable of developing the health of everyone [8].
Notes and references
Cover thumbnail. Image by mohamed_hassan from Pixabay.
[1] Horton, R. (2020) Offline: Covid-19 is not a pandemic. Lancet 396, 874.
[2] https://en.wikipedia.org/wiki/Merrill_Singer
[3] Wilson, P. et al. (2014) “Using Syndemic Theory to Understand Vulnerability to HIV Infection among Black and Latino Men in New York City.” Journal of Urban Health: 983-998
[4] Singer M, Bulled N, Ostrach B, Mendenhall E. (2017) Syndemics and the biosocial conception of health. The Lancet. 389:941-50.
[5] Courtin E, Vineis P. Covid-19 as a Syndemic. Front Public Health. 2021 Sep 9;9:763830. doi: 10.3389/fpubh.2021.763830. PMID: 34568273; PMCID: PMC8459739.
[6] Saltelli A. et al. (2020) Five ways to ensure that models serve society: a manifesto. Nature 582 (7813)
[7] https://www.senat.fr/rap/r21-537/r21-5371.pdf
[8] https://www.euro.who.int/__data/assets/pdf_file/0003/129675/Ottawa_Charter_F.pdf