Climate change: what effects on our health?
PDF
Between 2030 and 2050, climate change is expected to generate nearly 300,000 additional deaths per year, increasing child malnutrition and undernutrition, insect-borne diseases, diarrhoea and heat-related stresses. The potential influences of these changes on health are therefore multiple and interrelated. To these damages, it is necessary to add the migration of populations fleeing profound changes in their living environment: decrease in agricultural yields, floods, sea level rise…. Nearly 250 million “climate refugees” are expected at the horizon of 2050. Everyone remembers the excess of mortality in Europe during the heat wave in the summer of 2003, whereas 70,000 deaths were recorded in August alone. The climatic effects on infectious diseases are more complex. But entomologists are convinced that the expansion of hot and humid areas on the surface of the globe would increase populations of virus-carrying insects tenfold. Finally, the economic impacts of climate change speak for themselves: the estimated cost of direct health damage is estimated at between $2 billion and $4 billion per year by 2030.
- 1. An alarming observation
- 2. What are the effects on human health?
- 2.1. Deadly heat waves
- 2.2. Rising vector-borne infectious diseases
- 2.3. Natural disasters: what are the health effects?
- 2.4. What impact on water and food?
- 2.5. Impact of climate change on mental health – climate refugees
- 2.6. Microbes released by the melting of permafrost?
- 2.7. Biodiversity collapse and human health effects?
- 3. Conclusion: Health, climate change & global change
1. An alarming observation
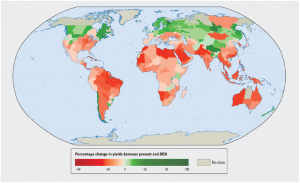
The temperature has increased by about 0.85°C worldwide over the past 130 years. This increase is mainly due to the increase in greenhouse gases. Over the past 25 years, the rate has accelerated and we are at more than 0.18°C of warming per decade [1]. Sea levels are rising, glaciers are melting and rainfall distribution is changing. In addition to these factual events, there are global climate changes, which are more complex to measure and which are manifested, among others, by extreme weather events (drought, floods, heat waves) increasing in intensity and frequency (see Tropical Cyclones: impacts and risks). Apart from a few rare effects of climate change that could be considered positive (e. g. reduction in winter mortality in temperate zones), these appear to be harmful to health. For example, the negative impacts of climate change on the yields of most crops can be cited. In their fifth assessment report [2], members of the IPCC (Intergovernmental Panel on Climate Change) noted many periods of very rapid increases in food and cereal prices following extreme weather events (giant fires, storms, floods).
This has (and will have) a very strong impact on the poorest populations, for whom the purchase of food has become very difficult. A 2009 report published by the British journal The Lancet [3] identified climate change as the greatest global threat to public health in the 21st century.On Thursday 29 November 2018, The Lancet published the second edition of its “Lancet Countdown” report dedicated to the health aspects of climate change. The result of collaboration between 27 academic institutions, UN and intergovernmental agencies from all continents, this document reveals the “unacceptable” risk to the current and future health of people around the world due to climate change.
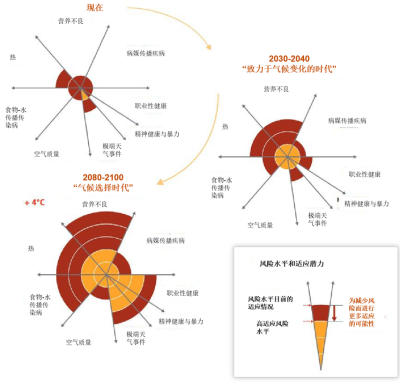
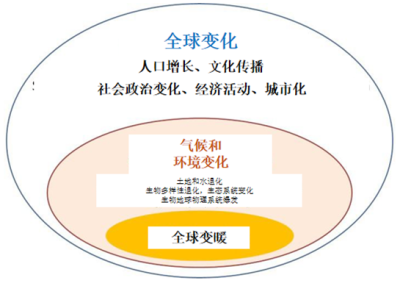
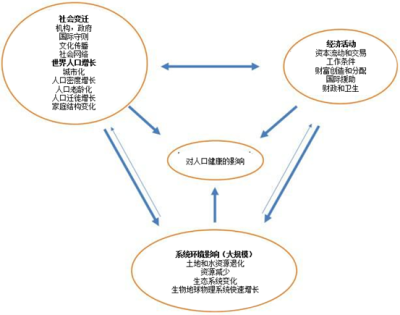
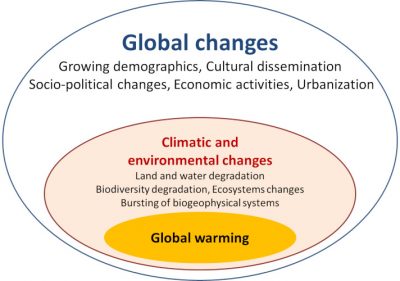
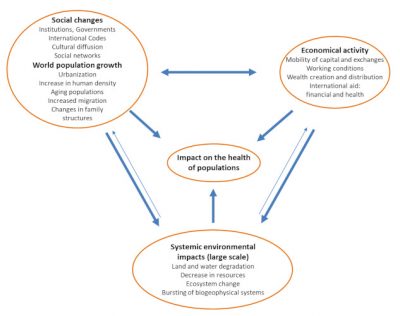
In conclusion, the effects of climate change are already being perceived today and projections for the future represent a potentially catastrophic risk of a magnitude that is difficult to accept for human health. Finally, the effects of global warming on human health are in addition to the effects of changes linked to globalization (demographic changes, social change, economic activity) [4].
2. What are the effects on human health?
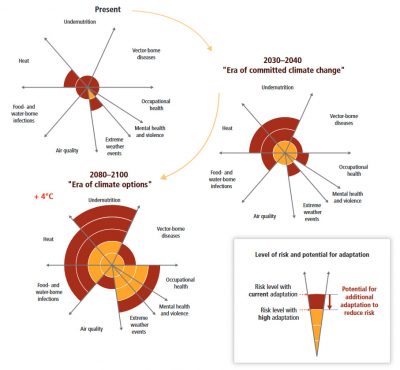
(a) direct effects: malnutrition and undernourishment (probably the most important), mortality and morbidity related to extreme events (heat waves), mortality and morbidity rates related to infectious diseases (vector transmissions and food and waterborne infections).
(b) indirect health effects: water availability, access to food, sea-level rise,…..
But many other diseases are linked to climate change:
(a) post-traumatic mental stress related to extreme events and resulting migration phenomena for climate refugees;
(b) respiratory pathologies related to air pollution, such as ozone content, which increases with temperature. Rising temperatures are also expected to increase allergies. more complex to assess in the context of climate change.
We will begin this inventory by citing some direct and undeniable effects (e.g. heat waves), then continue this chapter to more complex topics (e.g. malnutrition) associated with many factors beyond climate (including geopolitical and demographic) (Figure 2).
2.1. Deadly heat waves
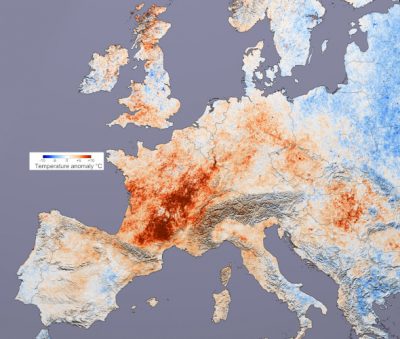
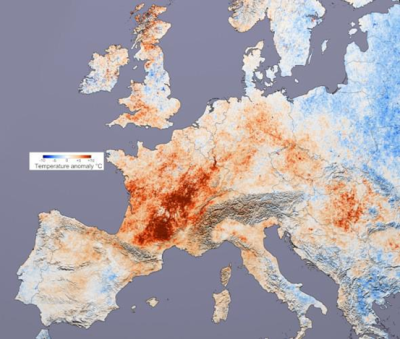
The 2003 European heat wave, which occurred from June to August, was a climatic event of exceptional magnitude. Marked by numerous temperature records during the first half of August, it would not have had an equivalent since the 16th century [5]. This heat wave had followed an exceptionally hot and dry spring with temperatures already reaching 30°C at the end of April in some places. Combined with a record dry spell, this heat wave is reminiscent of the summer 1947 heat wave in Europe and the 1976 drought (Figure 3). In some countries, such as France or Portugal, the consequences were significant on ecosystems, crop levels (-20% in France), population, and infrastructure… even causing a political crisis. Different sources (Inserm, INSEE, INED, France) converge today towards an estimate of about 15,000 excess deaths in France, i.e. an excess mortality of +55%! An excess of death observed mainly among the elderly. The most affected age group is the over 75 age group. At equal age, women were more affected than men. The signs reported were muscle cramps, heat exhaustion, heat stroke mortality (cardiovascular decompensation).
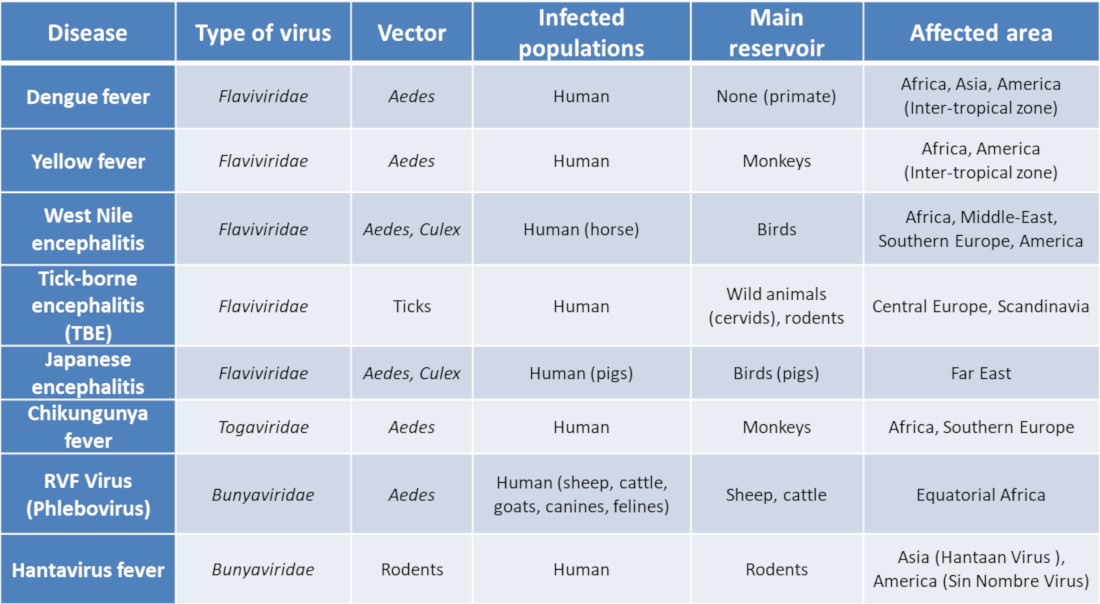
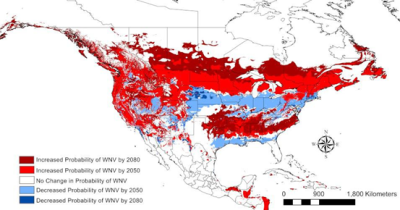
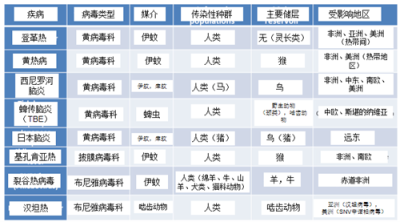
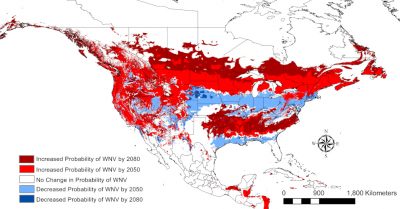
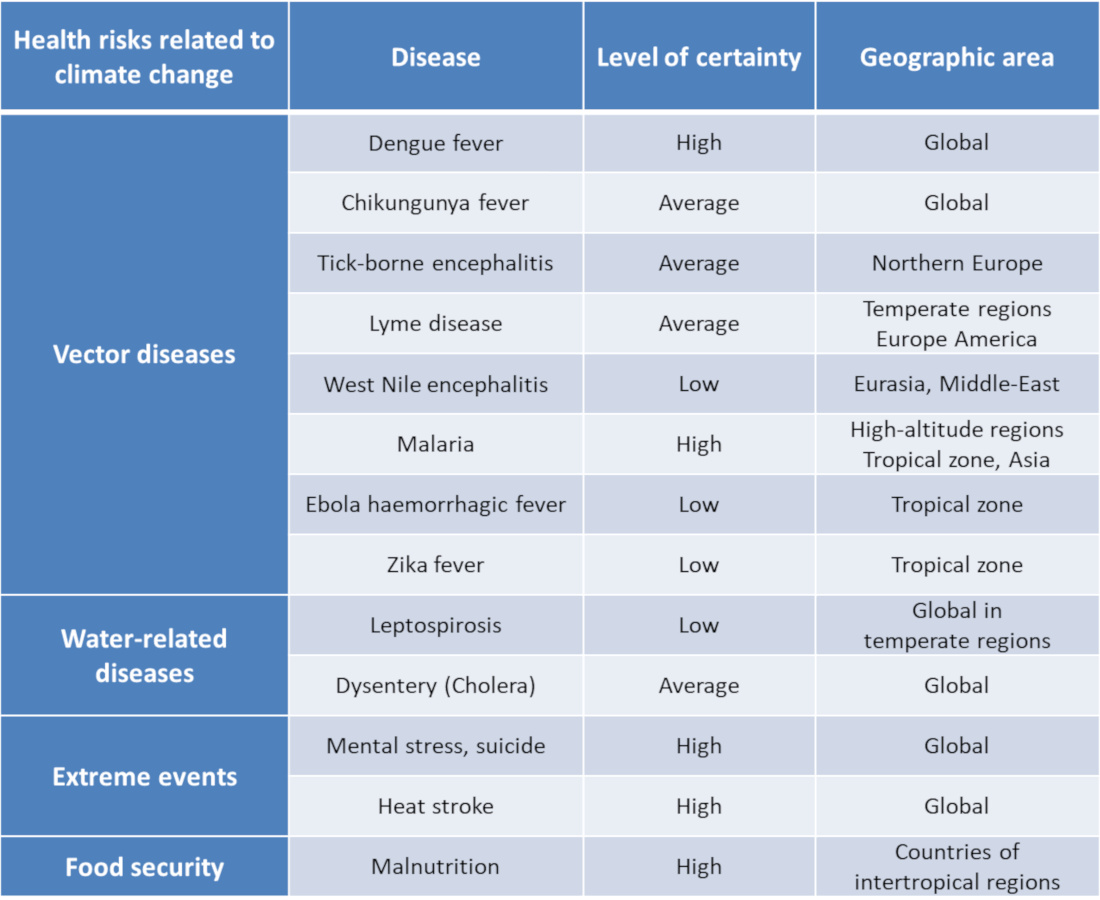
This heat wave will remain a reference point for previous and subsequent events of the same type. Other heat waves have since been recorded around the world, particularly in the USA during the summer of 2012 (Figure 4). The latter event, after a mild and rainy winter, has been associated with an increase in cases of West Nile encephalitis (viral encephalitis – West Nile Virus) [7] (see Table 1). A recent study [8] concludes that nearly one in three people in the world would be exposed to potentially fatal heat waves, a proportion that could rise to three in four by the end of the century, if greenhouse gas emissions continue at their current rate.
2.2. Rising vector-borne infectious diseases
2.2.1. General data
The expansion of insect vectors of infectious microbes is due to several factors: (i) The increase in winter temperatures would increase their period of activity (and therefore reproduction) and thus modify the epidemiological profile of mosquito and tick vector-borne diseases (continuous transmission due to a virtual absence of diapausePhase, genetically determined in the development of an organism, during which it reduces the intensity of its metabolic activities.). (ii) Droughts encourage the storage of water in tanks that are conducive to mosquito breeding. (iii) Rainfall in turn creates water points conducive to mosquito development.
In addition, the activity of ticks of the genus Ixodes reaches its maximum at mild temperatures. The frequency of encephalitisDiseases characterized by inflammation of the brain (brain, brainstem and/or cerebellum) transmitted by these insects is therefore expected to increase with global warming (see Table 1).
2.2.2. Some examples of vector-borne diseases
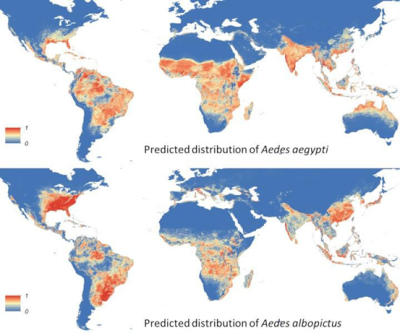
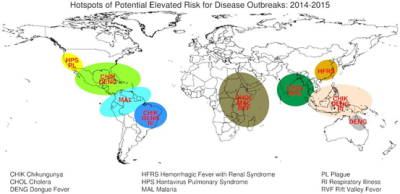
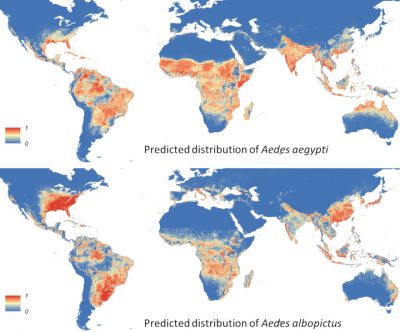
The first example of arbovirus whose incidence increases with global warming is Denguevirus [11]. This virus is transmitted by Aedes aegypti and Aedes albopictus, and the disease is observed in equatorial areas of America, Africa and Asia. The number of reported epidemics worldwide and cases in Europe [12] is increasing. According to the World Health Organization, approximately 2.5 billion people are now exposed to this risk; there are an estimated 50 million cases of Dengue fever and 500,000 cases of haemorrhagic dengue fever each year, including a high proportion of children requiring hospitalization. Experts estimate that an additional 3 billion people could be at risk of dengue fever transmission by the 2080s [13].
Carried by mosquitoes of the genus Culex, the West Nile Virus (WNV) is transmissible to birds and mammals, including humans. Its emergence in the USA in 1999 and its strong resurgence in 2012 argue for a role for climate change in this region of the globe (Table 1 and Figure 5). Since its introduction in North America, the virus has affected millions of Americans: 780,000 have fallen ill and more than 16,000 have developed encephalitis and 1549 have died from it [14].
For some viral diseases, the increase in the number of cases is due both to global warming and to phenomena related to global change. For example, in Latin America, deforestation and urbanization have changed the epidemiological characteristics of Dengue fever. This disease has evolved from an enzooticmode to an endemic{tooltip}mode. It characterizes a disease in animals whose incidence rate is generally quite stable and sylvatic (forest) to a mode endemicand characterizes a disease in humans whose incidence rate is generally quite stable and urban [15]. One may wonder whether the repetition on an increasing scale of severity (over time) of Ebola virus epidemics in Africa or the recent emergence of the Zika virus in Latin America could not be one of the consequences of climate change [16].
But there are other examples of mosquito-borne viruses of the genus Aedes:
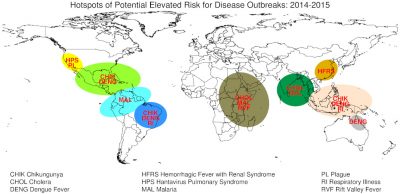
(i) Chikungunya virus infection has circulated widely in Africa and Asia (Figure 6). Characterized by febrile joint pain, its local transmission has increased in Italy. The mosquito vector is also widely present in France.
(ii) Rift Valley Fever Virus (RVFV) infection is responsible for livestock epizootics. Promiscuity between humans and animals has increased the number of cases, with an expansion to the north (Saudi Arabia) (Figure 6).
Regarding malaria agents (Plasmodium vivax and Plasmodium falciparum) carried by the Anopheles gambiae mosquito, epidemics have been observed in Kenya, particularly at altitudes above 2000 metres where temperatures exceed 18°C and rainfall exceeds 15 cm/month [17]. Immunologically naïve populations living in high altitude areas will be particularly exposed to malaria depending on the level of warming in these mountainous areas [18].
2.3. Natural disasters: what are the health effects?
Multiplying the number of storms and floods, the El Niño climatic phenomenon (ENSO or El Niño Southern Oscillation) is an important risk factor for infectious diarrhoea [19] and gastroenteritis due to Norovirus [20]. Aggravatingly, it causes population movements and promiscuity that can amplify inter-human transmissions, between humans and animals, and through contaminated water. Epidemic diarrhoea caused by the bacterium Vibrio cholerae, cholera has been particularly studied (see Figure 6). Indeed, through a series of measurements between 1980 and 1998, researchers noted that the incidence of cholera in Bangladesh followed seasonal variations correlated with temperature oscillations related to the El Niño phenomenon [21].
In both Bangladesh and Peru, cholera dynamics are indeed linked to El Niño oscillations; the latter seem to be linked in particular to the re-emergence of cholera in Peru in 1991, as bacteria settle on plankton and drift across the Pacific Ocean from west to east.
Another highlight in 2001-2002 was the emergence in Malaysia of the Nipah Virus, responsible for severe and fatal hemorrhagic fevers in 70% of cases. An event analysed as the joint action of a major El Niño phenomenon in 1998 and dramatic deforestation in this region of the world [22]. The virus was then transmitted by infected bats fleeing massively from the devastated forests. As they did not develop symptoms, they then easily contaminated mammals (e.g. pigs) and in particular humans.
Hantaviruses are another example of microorganisms that are sensitive to climatic variations, particularly extreme rainfall. They mainly cause two syndromes in humans: hemorrhagic fever with renal syndrome (in Asia and Europe), and cardiopulmonary syndrome (in North America) (Figure 6).
2.4. What impact on water and food?
2.4.1. Increasingly restricted access to water
The increasingly uncertain nature of precipitation is likely to have an impact on the supply of fresh water (see Are we at risk of water scarcity?). Lack of safe water can compromise hygiene and increase the risk of diarrhoeal diseases that kill nearly 600,000 children under the age of five each year. In extreme cases, water scarcity leads to drought and famine. And by 2090, climate change is expected to expand the areas affected by droughts, double the frequency of extreme droughts and increase their average duration by a factor of six [23].
Floods are also increasing in both frequency and intensity. They contaminate freshwater sources, increase the risk of water-borne diseases and create breeding grounds for larvae of disease-carrying insects such as mosquitoes (see above). They also cause drownings and physical trauma, damage to housing and disruption of health and care services.
2.4.2. Access to food and malnutrition
Rising temperatures, impacts of climate events (ecosystem degradation, damage to infrastructure and human settlements)… All these factors will have an impact on food production (Figure 7). A recent WHO study already mentions a decline in food production in many of the poorest regions, up to 50% by 2020 in some African countries [24]. These effects will be exacerbated by sea-level rise, and contamination (or salinization) of water supplies and agricultural land.
2.5. Impact of climate change on mental health – climate refugees
Co-recipients of the 2007 Nobel Peace Prize, Al Gore and IPCC experts predict an increase in stress-related diseases [26] (stress, suicide): the impacts of climate change on mental health have been proven during heat waves or exceptional droughts [27]. With an estimated 250 million climate refugees by 2050, these diseases will be exacerbated by population movements due to sea-level rise and the destruction of housing, medical facilities and other essential services [28]. Let us remember that more than half of the world’s population lives less than 60 km from the sea! Affected populations will be forced to move, which will increase various health risks, from mental health disorders to respiratory and digestive diseases.
In addition, a recent study [29] suggests that in the United States, rising temperatures would increase the suicide rate. The study, conducted by a team of researchers from Stanford University, used data on suicide rates in the United States between 1968 and 2004 and monthly suicide rates in Mexico between 1990 and 2010. By comparing these data with temperature and precipitation data in American counties – from a climate mapping tool called PRISM – they found a very consistent relationship between temperature increases and increased suicide risk.
2.6. Microbes released by the melting of permafrost?
In August 2016, a 12-year-old boy living in the Siberian tundra was evacuated from an anthrax epidemic area in Russia. He died in the hospital in the city of Salekhard, capital of the autonomous district of Iamalo-Nenetsia, while another 20 people were diagnosed with the disease. The death is well related to anthrax, an infectious disease caused by the bacterium Bacillus anthracis. The boy had the intestinal form of the disease, which was harder to diagnose. The infection has thus resurfaced in Western Siberia after 75 years of absence. This event occurs at a time when epidemiological studies suggest a role for permafrost melting in the release of bacteria from reindeer herds (1.5 million reindeer) decimated by the disease between 1897 and 1925 in Siberia, and buried in permafrost [30]. It is likely that current heat waves will lead to the release of anthrax spores (a form of bacterial resistance) from these landfill areas.
Global experts looking at this region of the globe (peri-arctic areas) particularly affected by global warming consider a dramatic increase in the incidence of other zoonotic infectious diseases (bacterial: brucellosis, Lyme disease, leptospirosis – viral: rabies, Hantavirus fever, tick-borne encephalitis, West Nile encephalitis) plausible [31].
2.7. Biodiversity collapse and human health effects?
One aspect that is not well addressed in global changes and their impacts on human health is the collapse of biodiversity as a whole (see Biodiversity is not a luxury but a necessity). While effects on insect populations and impacts on certain vertebrates such as birds can already be identified, effects on humans are much more difficult to assess. Yet alarming reports indicate that the loss of biodiversity will endanger economies, livelihoods, food security and the quality of life of people around the world [32]. According to other sources [33], the loss of biodiversity in man’s natural environment would have a cost to human health and well-being, a cost that is hidden and transmitted unscrupulously to future generations, but that can be assessed by economics. This cost is mainly due to two factors: on the one hand, the disappearance of biological materials useful to humans for food and health, and on the other hand, the disruption or even collapse of functional ecosystems leading to the loss of “ecosystem” goods and services.
Finally, the effects of climate change on the endogenous and environmental microorganisms that are the basis of life are largely unexplored. Specific studies on vertebrates show that an increase in temperature leads to a decrease in the biodiversity of their microbiome. Similarly, ocean acidification causes significant microbiome changes in some invertebrates such as sponges. Serious hypotheses point to the modification of the human intestinal microbiome (see Human microbiotas: allies for our health) and the emergence of dysbiosis (pathologies linked to the imbalance of the intestinal microbiome: e. g. inflammatory bowel diseases, obesity, diabetes) according to global changes (rapid urbanization, fast food diet, sedentary life disconnected from natural environments, massive antibiotic use, thermal stress).
3. Conclusion: Health, climate change & global change
In this chapter we have tried to show the most obvious effects of climate change on human health. Two points should be highlighted. First of all, the measurement of the health effects of climate change can only be very approximate, particularly on the gradual effects as opposed to extreme events such as heat waves (e. g. impact on vector-borne diseases). This is mainly due to the “unpredictable” nature of infectious agents.
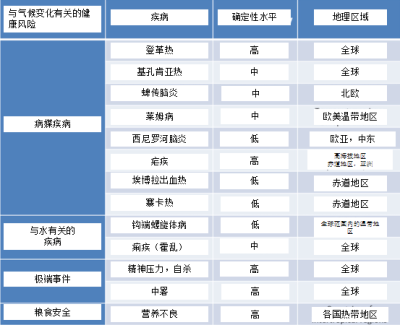
On the other hand, here is what we are certain about the impact of climate change on health [4]:
- Increase in the number of annual deaths or hospitalizations caused by heat stroke, both in rich and poor countries;
- Geographical extension of vector-borne infectious diseases or their vectors (e. g. high-altitude malaria);
- Increase in cholera epidemics in coastal areas linked to El Niño;
- Rising food prices, especially in countries suffering from precariousness, leading to food deprivation in low-income households (poverty traps).
Climate change will therefore have very negative impacts on health and the effects of global change will exacerbate them. All populations will feel the effects of climate change, but some are more vulnerable than others, for example:
- Those living in small island states, or in other coastal regions, megacities, mountainous regions and polar areas are particularly vulnerable.
- Children, especially those living in poor countries, are among the most vulnerable to the health risks that will result and will be exposed to the consequences for a longer period of time.
Health effects should also be more serious for the elderly and people with pre-existing disabilities or conditions.
Table 2. Summary of the health risks related to climate change.
According to WHO, areas without good health infrastructure, most of them in developing countries, will be the least able to prepare and cope with the situation without assistance. If a major mitigation effort is not undertaken, there will come a time when health systems adaptation (e.g. heat stroke) will no longer be possible. The only responsible attitude now would be a radical change in our economic models and lifestyles in society. It has become a matter of life and death, for humans and for the biodiversity on which their health depends very directly.
References and notes
[1] IPCC. Summary for Policymakers. In: Edenhofer O, R. Pichs-Madruga, Y. Sokona, E. Farahani, S. Kadner, K. Seyboth, A. Adler, I. Baum, S. Brunner, P. Eickemeier, B., Kriemann JS, S. Schlömer, C. von Stechow, T. Zwickel and J.C. Minx editors (2014), Climate Change 2014, Mitigation of Climate Change Contribution of Working Group III to the Fifth Assessment Report (AR5) of the Intergovernmental Panel on Climate Change. Cambridge, United Kingdom and New York, NY, USA, Cambridge University Press
[2] Smith KR et al (2014) Human Health: Impacts, adaptation, and co-benefits. In Climate change: Impacts, Adaptation, and vulnerability. Part A: Global and Sectoral aspects. Contribution of Working Group II to the 5th assessment Report (AR5) of the Intergovernmental Panel on Climate change. Field CB et al (eds), Cambridge University Press, UK pp 709-754
[3] Costello A et al (2009) Managing the health effects of climate change. Lancet 373: 1693-1733
[4] McMichael AJ (2013) Globalization, climate change and Human Health. New Engl J Med 368: 1335-1343
[5] Schär C (2004) The role of increasing temperature variability in European Summer heatwaves. Nature 427: 332-336
[6] Robine JM et al (2008) Death toll exceeded 70,000 in Europe during the summer of 2003. Reports/Biology Series, 331:171-78
[7] Wimberly et al (2014) Regional variation of climatic influences on West Nile virus Outbreaks in US. Am. J Too much. Med Hyg. 91: 677-684
[8] Mora C et al (2017) Global risk of deadly heat. Nature Climate Change. doi:10.1038/nclimate3322
[9] Zhang Y, Hansen A, Bi P. (2014) Climate change and vector-borne viral diseases. In Viral infections and global change. Singh SK ed John Wiley & sounds Hoboken, New Jersey
[10] Kraemer MU et al (2015) The global distribution of the arbovirus vectors Aedes aegypti and Ae. albopictus. Elife 4:e08347
[11] Hales S et al (2002) Potential effect of population and climate changes on global distribution of dengue fever: an empirical model. Lancet 360:830-4
[12] Schaffner F & Mathis A (2014). Dengue and dengue vectors in the WHO European region: past, present, and scenarios for te future. Lancet Infect Dis 14: 1271-1280
[13] Bhatt S et al (2013) The global distribution and burden of Dengue. Nature 496: 504-507
[14] Harrigan RJ et al (2014) A continental risk assessment of West Nile Virus under climate change. Global Change Biology 20: 2417-2425
[15] Weaver S (2013) Urbanization and geographic expansion of zoonotic arboviral diseases: mechanisms and potential strategies for prevention. Trends Microbiol. 21(8):360-3.
[16] Paz S. & Semenza J.C. (2016) El Niño and climate change-contributing factors in the dispersal of Zika virus in the Americas? Lancet 387(10020):745
[17] Jonathan A. Patz & William K. Reisen (2001) Immunology, climate change and vector-borne diseases. Trends in Immunology Vol.22 No.4 April 2001
[18] Lindsay S.W. & Martens W.J. (1998) Malaria in the African highlands: past, present and future. Bull World Health Organ. 76(1):33-45
[19] Pascual M. et al (2000) Model relationship between ENSO and cholera in Bangladesh (Int. Center For Diarrhoeal disease Research, Bangladesh) Science, 289(5485):1766-9.
[20] Chrétien J.P. et al (2015) Global climate anomalies and potential infectious disease risks. Plos Current outbreaks doi: 0.1371/currents.outbreaks.95fbc4a8fb4695e049baabfc2fc8289f
[21] Rodo X et al (2002) ENSO and cholera: a non stationary link related to climate change? Proc Natl Acad Sci USA 99(20):12901-6.
[22] Chua KB et al (2002) Anthropogenic deforestation, El Niño and the emergence of Nipah virus in Malaysia. Malays J Pathol. 24(1):15-21.
[23] Food Policy Report No. 21, September 2009. International Food Policy Research Institute (IFPRI) IPCC Fourth Assessment Report: Climate Change 2007 (AR4)
[24] WHO (2014) Quantitative risk assessment of the effects of climate change on selected causes of death, 2030s and 2050s. Geneva: World Health Organization
[25] Wheeler T & von Braun J. (2013) Climate change impacts on global food security. Science 2013;341:508-13
[26] Levy BS & Patz JA (2015) Climate change, Human rights and social justice. Annals Global Health 81, 3: 310-322
[27] Berry H.L., Bowen, K & Hjellstrom T. (2010) Climate change and mental health: a causal pathways framework. Int J Public Health. 55(2):123-32.
[28] Black R, Bennett SR, Thomas SM, Beddington JR (2011) Climate change: Migration as adaptation. Nature 478:447-9.
[29] Burke M et al (2018). Higher temperatures increase suicide rates in the United States and Mexico. Nature Climate change 8: 723-729
[30] Revich BA & Podolnaya MA (2011) Thawing of permafrost may disturb historic cattle burial grounds in east Siberia. Global Health Action doi: 10.3402/gha.v4i0.8482. Epub 2011 Nov 21
[31] Parkinson AJ, Evengard B, Semenza JC, et al (2014) Climate change and infectious diseases in the Arctic: establishment of a circumpolar working group. Int J Circumpolar Health. doi: 10.3402/ijch.v73.25163.) e(31
[32] https://www.who.int/globalchange/ecosystems/biodiversity/fr/
[33] http://sante-biodiversite.vetagro-sup.fr/wp-content/uploads/HB-REVUE2015HS_web-aout-20153.pdf
The Encyclopedia of the Environment by the Association des Encyclopédies de l'Environnement et de l'Énergie (www.a3e.fr), contractually linked to the University of Grenoble Alpes and Grenoble INP, and sponsored by the French Academy of Sciences.
To cite this article: DROUET Emmanuel (May 7, 2019), Climate change: what effects on our health?, Encyclopedia of the Environment, Accessed July 27, 2024 [online ISSN 2555-0950] url : https://www.encyclopedie-environnement.org/en/health/climate-change-what-effects-on-health/.
The articles in the Encyclopedia of the Environment are made available under the terms of the Creative Commons BY-NC-SA license, which authorizes reproduction subject to: citing the source, not making commercial use of them, sharing identical initial conditions, reproducing at each reuse or distribution the mention of this Creative Commons BY-NC-SA license.